Cirrhosis is a complication of many liver diseases. It is a chronic condition in which the liver slowly deteriorates and malfunctions due to chronic injury. Scar tissue replaces healthy liver tissue, partially blocking the flow of blood through the liver.
Scarring also impairs the liver’s ability to
- Control infections
- Remove bacteria and toxins from the blood
- Process nutrients, hormones, and drugs
- Make proteins that regulate blood clotting
- Produce bile to help absorb fats including cholesterol and fat-soluble vitamins
A healthy liver is able to regenerate most of its own cells when they become damaged. With end-stage cirrhosis, the liver can no longer effectively replace damaged cells. A healthy liver is necessary for survival.
Cirrhosis is the twelfth leading cause of death by disease, accounting for 27,000 deaths each year. The condition affects men slightly more often than women.
Causes
Cirrhosis has various causes. Cirrhosis is most commonly caused by alcoholism, hepatitis B and C, and fatty liver disease, but has many other possible causes. Some cases are idiopathic.
Obesity is becoming a common cause of cirrhosis, either as the sole cause or in combination with alcohol, hepatitis C, or both. Many people with cirrhosis have more than one cause of liver damage. Cirrhosis is not caused by trauma to the liver or other acute, or short-term, causes of damage. Usually years of chronic injury are required to cause cirrhosis.
Alcohol-related liver disease –
Most people who consume alcohol do not suffer damage to the liver. But heavy alcohol use over several years can cause chronic injury to the liver. The amount of alcohol it takes to damage the liver varies greatly from person to person. For women, consuming two to three drinks—including beer and wine—per day and for men, three to four drinks per day, can lead to liver damage and cirrhosis. In the past, alcohol-related cirrhosis led to more deaths than cirrhosis due to any other cause. Deaths caused by obesity-related cirrhosis are increasing.
Chronic hepatitis C –
The hepatitis C virus is a liver infection that is spread by contact with an infected person’s blood. Chronic hepatitis C causes inflammation and damage to the liver over time that can lead to cirrhosis.
Chronic hepatitis B and D –
The hepatitis B virus is a liver infection that is spread by contact with an infected person’s blood, semen, or other body fluid. Hepatitis B, like hepatitis C, causes liver inflammation and injury that can lead to cirrhosis. The hepatitis B vaccine is given to all infants and many adults to prevent the virus. Hepatitis D is another virus that infects the liver and can lead to cirrhosis, but it occurs only in people who already have hepatitis B.
Nonalcoholic fatty liver disease (NAFLD) –
In NAFLD, fat builds up in the liver and eventually causes cirrhosis. This increasingly common liver disease is associated with obesity, diabetes, protein malnutrition, coronary artery disease, and corticosteroid medications.
Autoimmune hepatitis –
This form of hepatitis is caused by the body’s immune system attacking liver cells and causing inflammation, damage, and eventually cirrhosis. Researchers believe genetic factors may make some people more prone to autoimmune diseases. About 70 percent of those with autoimmune hepatitis are female.
Diseases that damage or destroy bile ducts –
Several different diseases can damage or destroy the ducts that carry bile from the liver, causing bile to back up in the liver and leading to cirrhosis. In adults, the most common condition in this category is primary biliary cirrhosis, a disease in which the bile ducts become inflamed and damaged and, ultimately, disappear. Secondary biliary cirrhosis can happen if the ducts are mistakenly tied off or injured during gallbladder surgery. Primary sclerosing cholangitis is another condition that causes damage and scarring of bile ducts. In infants, damaged bile ducts are commonly caused by Alagille syndrome or biliary atresia, conditions in which the ducts are absent or injured.
Inherited diseases –
Cystic fibrosis, alpha-1 antitrypsin deficiency, hemochromatosis, Wilson disease, galactosemia, and glycogen storage diseases are inherited diseases that interfere with how the liver produces, processes, and stores enzymes, proteins, metals, and other substances the body needs to function properly. Cirrhosis can result from these conditions.
Drugs, toxins, and infections –
Other causes of cirrhosis include drug reactions, prolonged exposure to toxic chemicals, parasitic infections, and repeated bouts of heart failure with liver congestion.
Symptoms
Many people with cirrhosis have no symptoms in the early stages of the disease. However, as the disease progresses, a person may experience the following symptoms:
- Loss of appetite
- Lack of energy (fatigue), which may be debilitating
- Nausea, vomiting
- Weight loss or sudden weight gain
- Bruises
- Yellowing of skin or the whites of eyes (jaundice)
- Itchy skin
- Fluid retention (edema) and swelling in the ankles, legs, and abdomen (often an early sign)
- Abdominal pain and bloating
- Spiderlike blood vessels on the skin
- A brownish or orange tint to the urine
- Light colored stools
- Confusion, disorientation, personality changes
- Blood in the stool
- Fever
Complications
As liver function deteriorates, one or more complications may develop. In some people, complications may be the first signs of the disease.
Edema and ascites –
When liver damage progresses to an advanced stage, fluid collects in the legs, called edema, and in the abdomen, called ascites. Ascites can lead to bacterial peritonitis, a serious infection.
Bruising and bleeding –
When the liver slows or stops producing the proteins needed for blood clotting, a person will bruise or bleed easily.
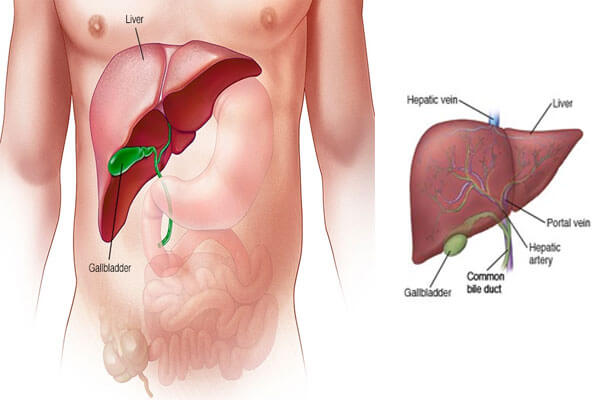
Portal hypertension –
Normally, blood from the intestines and spleen is carried to the liver through the portal vein. But cirrhosis slows the normal flow of blood, which increases the pressure in the portal vein. This condition is called portal hypertension.
Esophageal varices and gastropathy –
When portal hypertension occurs, it may cause enlarged blood vessels in the esophagus, called varices, or in the stomach, called gastropathy, or both. Enlarged blood vessels are more likely to burst due to thin walls and increased pressure. If they burst, serious bleeding can occur in the esophagus or upper stomach, requiring immediate medical attention.
Splenomegaly –
When portal hypertension occurs, the spleen frequently enlarges and holds white blood cells and platelets, reducing the numbers of these cells in the blood. A low platelet count may be the first evidence that a person has developed cirrhosis.
Jaundice –
Jaundice occurs when the diseased liver does not remove enough bilirubin from the blood, causing yellowing of the skin and whites of the eyes and darkening of the urine. Bilirubin is the pigment that gives bile its reddish-yellow color.
Gallstones –
If cirrhosis prevents bile from flowing freely to and from the gallbladder, the bile hardens as gallstones.
Sensitivity to medications –
Cirrhosis slows the liver’s ability to filter medications from the blood. When this occurs, medications act longer than expected and build up in the body. This causes a person to be more sensitive to medications and their side effects.
Hepatic encephalopathy –
A failing liver cannot remove toxins from the blood, and they eventually accumulate in the brain. The buildup of toxins in the brain—called hepatic encephalopathy—can decrease mental function and cause coma. Signs of decreased mental function include confusion, personality changes, memory loss, trouble concentrating, and a change in sleep habits.
Insulin resistance and type 2 diabetes –
Cirrhosis causes resistance to insulin—a hormone produced by the pancreas that enables the body to use glucose as energy. With insulin resistance, the body’s muscle, fat, and liver cells do not use insulin properly. The pancreas tries to keep up with the demand for insulin by producing more, but excess glucose builds up in the bloodstream causing type 2 diabetes.
Liver cancer –
Hepatocellular carcinoma is a type of liver cancer that can occur in people with cirrhosis. Hepatocellular carcinoma has a high mortality rate, but several treatment options are available.
Other problems –
Cirrhosis can cause immune system dysfunction, leading to the risk of infection. Cirrhosis can also cause kidney and lung failure, known as hepatorenal and hepatopulmonary syndromes.
Diagnosis
The diagnosis of cirrhosis is usually based on the presence of a risk factor for cirrhosis, such as alcohol use or obesity, and is confirmed by physical examination, blood tests, and imaging. The steps in making the diagnosis of cirrhosis will include medical analysis of the following:
During a physical examination the health care provider may find:
- An enlarged liver or spleen
- Excess breast tissue
- Expanded (distended) abdomen, as a result of too much fluid
- Reddened palms
- Red spider-like blood vessels on the skin
- Small testicles
- Widened (dilated) veins in the abdomen wall
- Yellow eyes or skin (jaundice)